More Stories
A Seaford couple says a change in Medicare coverage of a breast cancer screening test puts tens of thousands of women’s lives at risk.
Michael and Amy Gillman say it all started when Amy went in for her annual breast ultrasound test in June to check for breast cancer. Their radiologist told them about an unexpected change in Medicare coverage.

"They'd no longer be paid by Medicare for the breast ultrasound, and we had to promise to pay the fee, whatever it might be, for the ultrasound knowing in advance that Medicare would not pay for it,” said Michael Gillman.
Michael says for the last seven years, they’ve never had a problem and never were notified about the change prior.
"Medicare had covered the service in full. They no longer do so. This was quite a shock,” he said.
Amy gets an ultrasound in place of a mammogram because doctors say she has dense breasts, which make it harder for mammograms alone to detect cancer.
Stony Brook Medicine Chief of Breast Radiology Dr. Cindy Lee says Amy is not alone. Lee says women should start getting checked for breast cancer by at least age 40. She says half the women in the U.S. have dense breasts and ultrasounds are the best ways to detect cancer early in those women.
"With the ultrasound added on, in addition to the mammogram, you can find an additional two to four cancers for every 1,000 women we screen,” she said. “It's really adding a lot of that additional cancer detection."
Lee says Medicare’s coverage change puts thousands of women at risk for developing breast cancer since this method of preventative screening isn’t fully covered anymore by Medicare.
Gillman says Medicare told them the test would be covered, but only in specific circumstances.


"They won't pay for it until the woman already has signs of cancer,” he said. “This is not what a screening test is for. Breast cancer must be diagnosed before it has symptoms."
As he awaits a response from the AARP and Medicare about the change, he has a few questions for Medicare administrators.
"Is human life so worthless that you really feel that this is the way to go,” he said. "How can you deny a test that is known to diagnose cancer early enough to be easily treatable to tens of thousands of women who need it?"
Lee says people should check with any supplementary insurance plans to see if they’ll cover the procedure as a preventative measure. She also says people with questions about why the change happened should reach out to their congressional representatives and have them urge Medicare to cover ultrasounds.
While the cost varies depending on people's insurance plans, the Gillmans say it would cost them hundreds of dollars out-of-pocket to pay for the procedure.
More from News 12
1:32

beWell: Proactive and empowering breast cancer awareness info
2:12
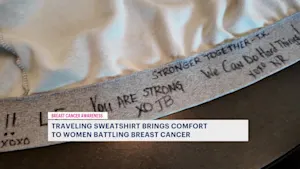
A hoodie and hope: New Jersey women share sweatshirt to bring comfort during breast cancer treatment
2:30

DiCuore Diamonds founder Daniela Sokolowski's breast cancer survival story
4:45

Actress brings real-life experience with BRCA gene, genetic testing to 'Love Danielle'
2:52

'Hamilton' & 'Wicked' star Mandy Gonzalez opens up about breast cancer journey
4:18
